- Have any questions?
- +380 (50) 50 73 903
- uapothecary.pharmacy@gmail.com
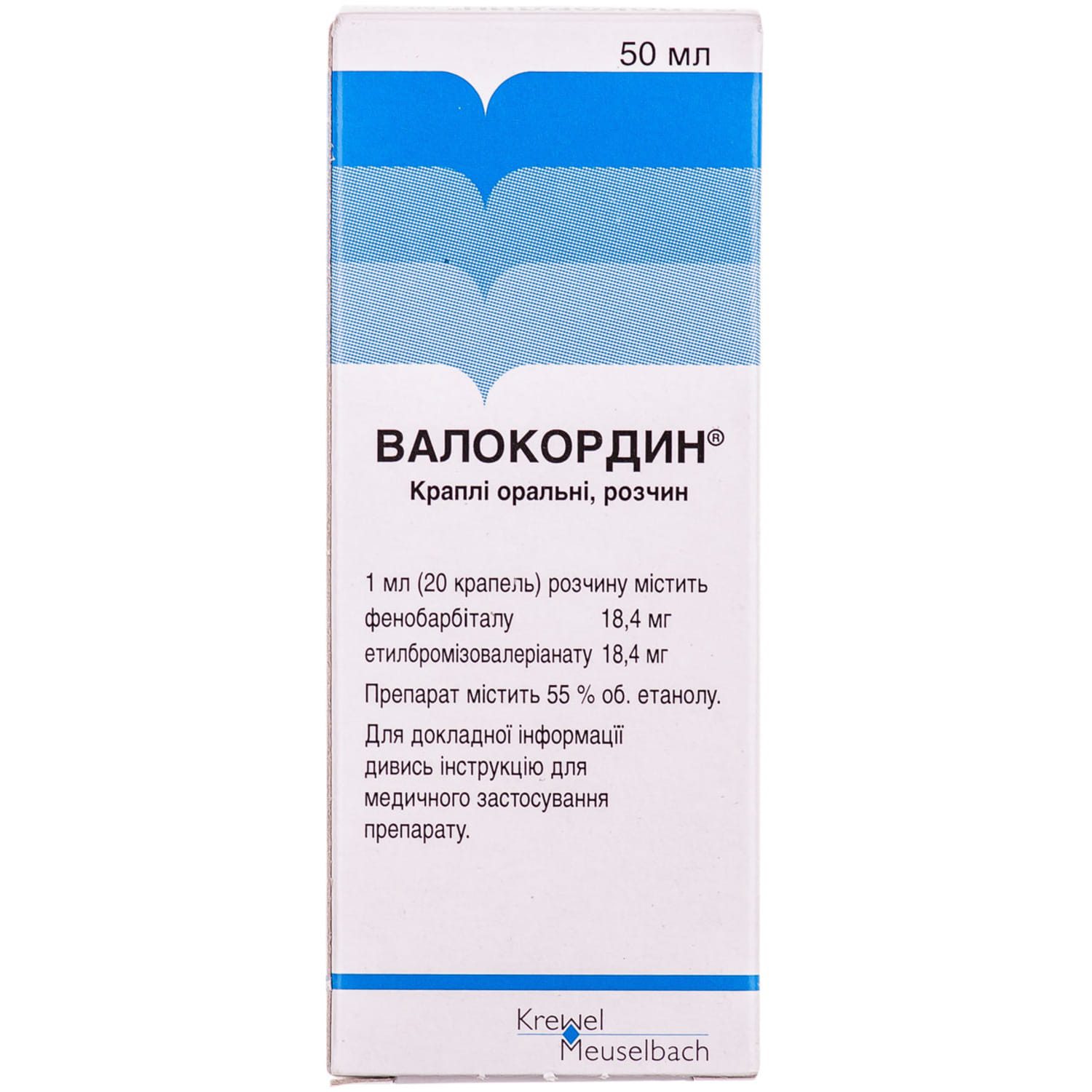
Valocordin oral drops dropper bottle 50 ml
$17.19
Valocordin is a combined drug, the effect of which is determined by the properties of the substances included in its composition. Has a sedative and antispasmodic effect. Facilitates the onset of natural sleep.
Ethyl ether of α-bromosovaleric acid causes a sedative (similar to valerian) and antispasmodic effect.
Phenobarbital enhances the sedative effect of other components and has a mild hypotensive effect.
Pharmacological properties
Pharmacodynamics. Valocordin is a combined drug containing phenobarbital and ethyl bromisovalerianate (ethyl ester of α-bromisovaleric acid). depending on the dose, both of these substances have a sedative, hypnotic effect, and in high doses – a narcotic effect. Like other derivatives of barbituric acid, phenobarbital inhibits the inhibitory system of reticular formation. ethyl bromisovalerianate has both antispasmodic and sedative effects. at the concentration contained in valocordin, ethyl bromisovalerianate acts as a synergist of phenobarbital (rapid manifestation of the effect).
Pharmacokinetics. Phenobarbital is absorbed quickly (directly in the stomach). About 35% binds to blood plasma proteins, the part that is not bound to proteins is filtered in the kidneys. Reabsorption occurs at a low pH level. Back diffusion does not occur due to the alkalinity of urine. Approximately 30% of phenobarbital is excreted unchanged in the urine, and only a small part of it is oxidized in the liver. With long-term use, there is an accumulation of the active substance in the blood plasma, as well as induction of liver enzymes. As a result of this induction, the oxidation of phenobarbital and other drugs is accelerated.
Bromine from ethyl bromisovalerianate is excreted very slowly from the body. If the drug is used for a long time, it accumulates in the central nervous system, which leads to chronic bromine intoxication.
Indication
Functional disorders of the cardiovascular system; neuroses accompanied by increased irritability and a sense of fear; psychosomatically caused anxiety; states of excitement with pronounced vegetative manifestations; sleep disturbance.
Application
It is prescribed for adults. used internally during meals with a small amount of liquid. the usual dose is 15-20 drops 3 times a day, with insomnia it can be increased to 30 drops. the duration of taking the drug is determined by the doctor.
Contraindication
Hypersensitivity to active substances or to any component of the drug, acute hepatic porphyria, severe liver and kidney dysfunction, diabetes, depression, myasthenia gravis. medicinal products containing phenobarbital are contraindicated in cases of alcoholism, drug and drug addiction (including history), respiratory diseases with shortness of breath, obstructive syndrome, pronounced arterial hypotension, acute myocardial infarction, depressive disorders with a patient’s tendency to suicidal behavior .
Side effects
On the part of the nervous system: asthenia, weakness, impaired coordination of movements, nystagmus, ataxia, hallucinations, paradoxical excitement, insomnia (in elderly patients), decreased concentration of attention, fatigue, inhibition of reactions, headache, cognitive impairment. in some cases, drowsiness and slight dizziness, confusion of consciousness may be noted.
On the part of the musculoskeletal system: with long-term use of drugs containing phenobarbital, there is a risk of osteogenesis disorder and rickets. Decreased bone mineral density, osteopenia, osteoporosis, and fractures have been reported in patients receiving long-term phenobarbital therapy. The mechanism by which phenobarbital affects the metabolism of bone tissue has not been established.
Gastrointestinal tract: nausea, vomiting, constipation, heaviness in the epigastric region, with long-term use – impaired liver function.
From the hematopoietic organs: agranulocytosis, megaloblastic anemia, thrombocytopenia, anemia.
From the side of the cardiovascular system: a decrease in blood pressure, bradycardia.
Very rarely: allergic reactions, including angioedema, difficulty breathing, facial swelling, rash, itching.
Severe skin adverse reactions that have been reported when using phenobarbital: Stevens-Johnson syndrome and toxic epidermal necrolysis, urticaria, Lyell’s syndrome, rhinitis, conjunctivitis, acne, purpura, lacrimation.
Special instructions
Life-threatening skin reactions in Stevens-Johnson syndrome and toxic epidermal necrolysis have been reported with phenobarbital.
Patients should be warned of signs and symptoms and closely monitored for skin reactions. The highest risk of developing Stevens-Johnson syndrome or toxic epidermal necrolysis is noted during the first weeks of treatment.
If symptoms of Stevens-Johnson syndrome or toxic epidermal necrolysis (e.g. progressive skin rash, often with blisters and mucosal damage) occur, treatment should be discontinued.
The best results in the treatment of Stevens-Johnson syndrome or toxic epidermal necrolysis have been noted in the case of early diagnosis and immediate discontinuation of any drug suspected of causing these symptoms.
If the patient developed Stevens-Johnson syndrome or toxic epidermal necrolysis when using Valocordin, these patients should not use the drug in the future.
If the pain in the area of the heart does not go away after taking the drug, you should consult a doctor to rule out acute coronary syndrome. It is prescribed with caution in hyperkinesis, hyperthyroidism, hypofunction of the adrenal glands, uncompensated heart failure, severe arterial hypotension and constant pain, acute drug intoxication.
Valocordin contains 55 vol.% ethanol.
Long-term use of Valocordin is not recommended due to the risk of drug addiction, possible accumulation of bromine in the body and the development of bromine poisoning.
Children. There is no experience of using the drug in children.
The period of pregnancy and breastfeeding. During pregnancy and breastfeeding, taking the drug is contraindicated.
The ability to influence the speed of reaction when driving a motor vehicle or working with other mechanisms. Valocordin reduces the reaction rate. Patients taking Valocordin should refrain from potentially dangerous activities that require increased attention and speed of psychomotor reactions.
Interactions
When using the drug with other drugs that depress the central nervous system, mutual strengthening of the action (sedative-hypnotic effect) is possible, which may be accompanied by respiratory depression. alcohol enhances the effect of the drug and can increase its toxicity.
Medicinal products containing valproic acid enhance the effect of barbiturates.
Phenobarbital induces liver enzymes and, accordingly, can accelerate the metabolism of some drugs that are metabolized by liver enzymes (for example, coumarin derivatives, antibiotics, and sulfonamides). Phenobarbital enhances the effect of analgesics, anesthetics, anesthetics, neuroleptics, tranquilizers; reduces the effect of paracetamol, indirect anticoagulants, metronidazole, tricyclic antidepressants, salicylates, digitoxin.
Possible influence on the blood concentration of phenytoin, as well as carbamazepine and clonazepam. MAO inhibitors prolong the effect of phenobarbital. Rifampicin may reduce the effect of phenobarbital. When used with gold preparations, the risk of kidney damage increases. With long-term simultaneous use with non-steroidal anti-inflammatory drugs, there is a risk of stomach ulcers and bleeding. The simultaneous use of drugs containing phenobarbital with zidovudine increases the toxicity of both drugs. The interaction of Valocordin (containing phenobarbital) with lamotrigine, thyroid hormones, doxycycline, chloramphenicol, antifungal drugs (azole group), griseofulvin, GCS, oral contraceptives is undesirable due to the possible weakening of the action of these drugs.
Increases the toxicity of methotrexate.
Overdose
Symptoms acute (from mild to moderate) poisoning with barbiturates: dizziness, fatigue, deep sleep from which the patient cannot be awakened.
Hypersensitivity reactions may occur: angioedema, urticaria, itching, rash.
Acute severe poisoning: deep coma accompanied by tissue hypoxia, shallow breathing, first accelerated and then slowed down, increased heart rate, arrhythmia, hypotension, bradycardia, vascular collapse, reduction or loss of reflexes, nystagmus, headache, nausea, weakness, heart failure activity, a decrease in body temperature, a decrease in heart rate, a decrease in diuresis.
Failure to provide timely medical assistance may result in death as a result of vascular insufficiency, respiratory paralysis, or pulmonary edema.
Long-term use of drugs containing bromine can lead to bromine poisoning, which is characterized by the following symptoms: confusion, ataxia, apathy, depressed mood, conjunctivitis, colds, acne or purpura.
Treatment. Cases of acute valocordin poisoning should be treated in the same way as poisoning with other hypnotics and barbiturates, depending on the severity of the symptoms of poisoning. The patient must be hospitalized in the intensive care unit. Breathing and blood circulation require stabilization. Respiratory failure requires artificial respiration, shock is stopped by the administration of plasma and plasma substitutes. If a lot of time has passed after taking the drug, it is necessary to wash the stomach (inject 10 g of activated carbon powder and sodium sulfate into the stomach). In order to quickly remove barbiturates from the body, it is possible to carry out forced diuresis with alkalis, as well as hemodialysis and / or hemoperfusion.
Treatment of bromine poisoning: the removal of bromine ions from the body can be accelerated by the introduction of a significant amount of table salt solution with the simultaneous introduction of saluretic agents.
In the event of hypersensitivity reactions, prescribe desensitizing drugs.
Storage conditions
In the original packaging at a temperature not higher than 25 °C.
Current information
Valocordin is a combined drug with a predominantly sedative effect. it also has some hypnotic and antispasmodic effect. its therapeutic effect is explained by the synergistic effect of the components included in its composition. valocordin is a drug known since the 1950s, when it began to be produced and used in Germany in the treatment of functional and psychosomatic diseases of the cardiovascular system (koll jf, louis a., 1957), in patients with neuroses, neurotic disorders , increased anxiety, excitement, accompanied by expressed vegetative reactions, a sense of fear and increased irritability (marshall w., 1956). Valocordin appeared on the territory of the USSR in 1963 and soon gained popularity. despite the successes of the pharmaceutical industry and the lack of an evidence base about its effectiveness and safety, the drug is quite common.
Therapeutic effects of the active ingredients of the drug Valocordin
phenobarbital
According to the ATS classification, it belongs to antiepileptic drugs from the group of barbiturates. Previously, phenobarbital was widely used for the treatment of neuroses, insomnia and to relieve anxiety (Rickels K., Downing RW, 1974). Barbiturates, in particular phenobarbital, have a wide range of clinical applications, but today they are most often used as anticonvulsant therapy (Suddock JT, Cain MD., 2018). Phenobarbital is also recommended for the treatment of status epilepticus (Falco-Walter JJ, Bleck T., 2016). As a result of a study conducted in China, it was found that intravenous phenobarbital demonstrated a better clinical outcome in the treatment of status epilepticus than valproic acid (Su Y. et al., 2016). Despite this, its widespread use is limited by side effects (Hocker S. et al., 2018). Due to its anticonvulsant and sedative properties, phenobarbital is also used in the treatment of alcohol withdrawal syndrome along with benzodiazepines (Oks M. et al., 2018). But still, in the case of alcohol withdrawal syndrome, it is not the drug of choice, because according to numerous studies, benzodiazepines in this case demonstrate better effectiveness with fewer side effects (Hammond DA et al. 2017). Phenobarbital can be used to treat insomnia, but it is known to be addictive when used as a hypnotic (Gupta RN, 1985). Phenobarbital reduces intracranial pressure. However, this drug can cause hypotension, adversely affecting the supply of oxygen to the brain, so it is contraindicated in the treatment of craniocerebral injuries. In this case, hypoxia of the brain occurs, nullifying any clinical benefit of phenobarbital (Roberts I., Sydenham E., 2012).
The mechanism of action of phenobarbital is associated with an increase in the number of open ion chloride channels in GABA receptors (the outflow of chlorine ions increases), this leads to an increase in the sensitivity of these receptors to GABA. Thus, phenobarbital has a non-selective depressant effect on the central nervous system. It hyperpolarizes the cell membrane, thereby raising the threshold for the occurrence of an action potential. This mechanism explains its anticonvulsant effect (Suddock JT, Cain MD, 2018).
Phenobarbital is hydrophilic, its metabolism takes place in the liver. It is excreted mainly by the kidneys (Suddock JT, Cain MD, 2018). Phenobarbital induces cytochrome P450, this must be taken into account when prescribing with oral contraceptives. Due to the induction of cytochrome P450, phenobarbital accelerates the metabolism of estrogens and progestins, which means that it weakens the effect of oral contraceptives, which can lead to unwanted pregnancy (Sabers A., 2008). Phenobarbital has been shown in studies to reduce the levels of steroids and theophylline through the P450 metabolism system (Sayer WJ, 1975). Thus, patients who receive combined oral treatment in connection with lung pathology may experience the ineffectiveness of lung disease therapy associated with subtherapeutic levels of theophylline and/or corticosteroids in the blood. Patients must be informed about the potential risks of taking Valocordin before starting therapy.
Ethyl bromisovalerianate
This is the active substance of Valocordin, which acts as a synergist of phenobarbital. It has a sedative effect, some hypnosis mainly due to a general decrease in excitability and anxiety (Nosal M.A., Nosal I.M., 1960). Ethylbromisovalerianate also has an antispasmodic effect (Pastushenkov L.V., 1989).
Peppermint oil
Peppermint oil, as an auxiliary substance included in the composition of the drug Valocordin, has a mild vasodilator property. It also has a sedative and antispasmodic effect. In addition, in folk medicine it is used as a choleretic and antiemetic agent, reduces the likelihood of nausea and increased acidity of gastric juice (Nosal M.A., Nosal I.M., 1960).
hop oil
It has calming, sedative, anticonvulsant, analgesic and antispasmodic properties (Pastushenkov L.V. et al., 1990). In phytotherapy, it is used not only as a mild sedative, but also for the treatment of insomnia, inflammatory diseases of the stomach, gall bladder, and liver (Nosal, M.A., Nosal, I.M., 1960), and topically to relieve itching and pain in skin diseases.
Peppermint oil and hop oil in the Valocordin preparation are contained in small concentrations and are not components that mainly determine its therapeutic effect.
Side effects and possible complicationsSide effects and complications when taking Valocordin more often occur with uncontrolled use, overdose, duration of administration and / or self-medication.
The most common side effects are impaired coordination of movements, drowsiness, loss of appetite, depressed mood, irritability, pain in bones, joints and muscles, less often – liver damage, breathing disorders and coma. Both cases of Steven-Johnson syndrome when taking phenobarbital and fixed polymorphic bullous erythema when taking Valocordin are described (Savcak VI, 1987).
Elderly patients are especially prone to side effects. There is information on the treatment of 61 elderly and senile patients due to poisoning with phenobarbital, which is part of Valocordin. It was established that acute phenobarbital poisoning in elderly and senile patients is more often accompanied by the development of complications from the central nervous system, respiratory (pneumonia) and cardiovascular system than in younger patients. Also, such patients often have a more severe clinical course and a higher risk of developing an adverse outcome, poisoning (Livanov GA et al., 2018).
The risk of complications in patients with COPD is also higher (Suddock JT, Cain MD, 2018).
It is strictly forbidden to drink alcohol while taking barbiturates and combined drugs containing substances of this group. This is due to the fact that there is a possibility of suppression of the respiratory center. Alcohol enhances the inhibitory effect of phenobarbital on the central nervous system. Valocordin is not recommended for patients with chronic alcoholism or drug addiction.
It is also necessary to warn patients who take Valocordin about a possible decrease in the speed of reactions and impaired coordination. This is especially important when driving vehicles or working with other mechanisms.
It is not recommended to use Valocordin for patients with depression, as phenobarbital can increase its manifestations.
With uncontrolled intake of the drug, a significant excess of the dose, the development of the toxic effect of phenobarbital is possible.
Its symptoms include cognitive impairment, dizziness, muscle weakness, polydipsia, oliguria, hypothermia (lower body temperature), mydriasis, nausea, vomiting, bradycardia, and respiratory depression. The severity of these symptoms can vary significantly (Suddock JT, Cain MD, 2018).
The development of coma and death due to severe respiratory depression and hypotension are possible.
Valocordin with long-term use due to the content of phenobarbital contributes to the progression of osteoporosis. It is necessary to be careful and not to prescribe long-term Valocordin to patients with osteoporosis.
With long-term use of the drug in high doses, addiction is possible, as well as the development of a withdrawal syndrome when the drug is stopped.
In this regard, in some countries, for example, in the USA, the UAE and Estonia, Valocordin as a drug containing phenobarbital is included in the list of drugs prohibited for import into the country.
In case of overdose, the treatment is symptomatic. Therapy depends on the symptoms and their severity, may include respiratory support (intubation and mechanical ventilation), correction of bradycardia and hypotension (prescription of vasopressors, intravenous colloid and crystalloid solutions to restore fluid volume), forced diuresis or hemodialysis (Palmer BF, 2000) .
conclusionsValocordin is a drug with more than half a century of history. Today, it is also used as a sedative medicine to relieve cardialgia, insomnia, excitement, anxiety, and restlessness. However, patients should be informed about the possibility of serious side effects when abusing this drug. Therefore, it is necessary to remember that the composition of the drug includes phenobarbital, which has a wide range of undesirable side effects, as well as the development of addiction, withdrawal syndrome, toxic lesions, and even acute poisoning with phenobarbital in case of an overdose of Valocordin. Patients should be warned about possible drug interactions, as phenobarbital can reduce the therapeutic effect of many drugs, including indirect anticoagulants and some antibiotics and antifungal drugs. Women of reproductive age who use oral contraceptives should be warned about the weakening of their effect when used simultaneously with this drug. It is also necessary to remember that during the use of Valocordin, the use of alcohol is strictly prohibited due to the strengthening of the toxic effects of phenobarbital and depression of the central nervous system. It is not recommended to use the drug together with other sedative drugs, tranquilizers and neuroleptics due to their synergistic depressant effect on the central nervous system. Do not use the drug during pregnancy and breastfeeding. In case of compliance with all recommendations, prescribed dose and regimen, Valocordin is generally well tolerated.






Reviews
There are no reviews yet.