No products in the cart.
We deliver to:
🇦🇺 Australia
🇨🇦 Canada
🇨🇿 Czechia
🇩🇰 Denmark🇪🇪 Estonia
🇮🇪 Ireland
🇮🇱 Israel
🇮🇹 Italy
🇯🇵 Japan
🇲🇽 Mexico
🇵🇱 Poland
🇰🇷 South Korea
🇨🇭 Switzerland
🇬🇧 United Kingdom
🇺🇸 United States of Americaand more
We deliver to:
🇦🇺 Australia
🇨🇦 Canada
🇨🇿 Czechia
🇩🇰 Denmark🇪🇪 Estonia
🇮🇪 Ireland
🇮🇱 Israel
🇮🇹 Italy
🇯🇵 Japan
🇲🇽 Mexico
🇵🇱 Poland
🇰🇷 South Korea
🇨🇭 Switzerland
🇬🇧 United Kingdom
🇺🇸 United States of Americaand more
[category_image]
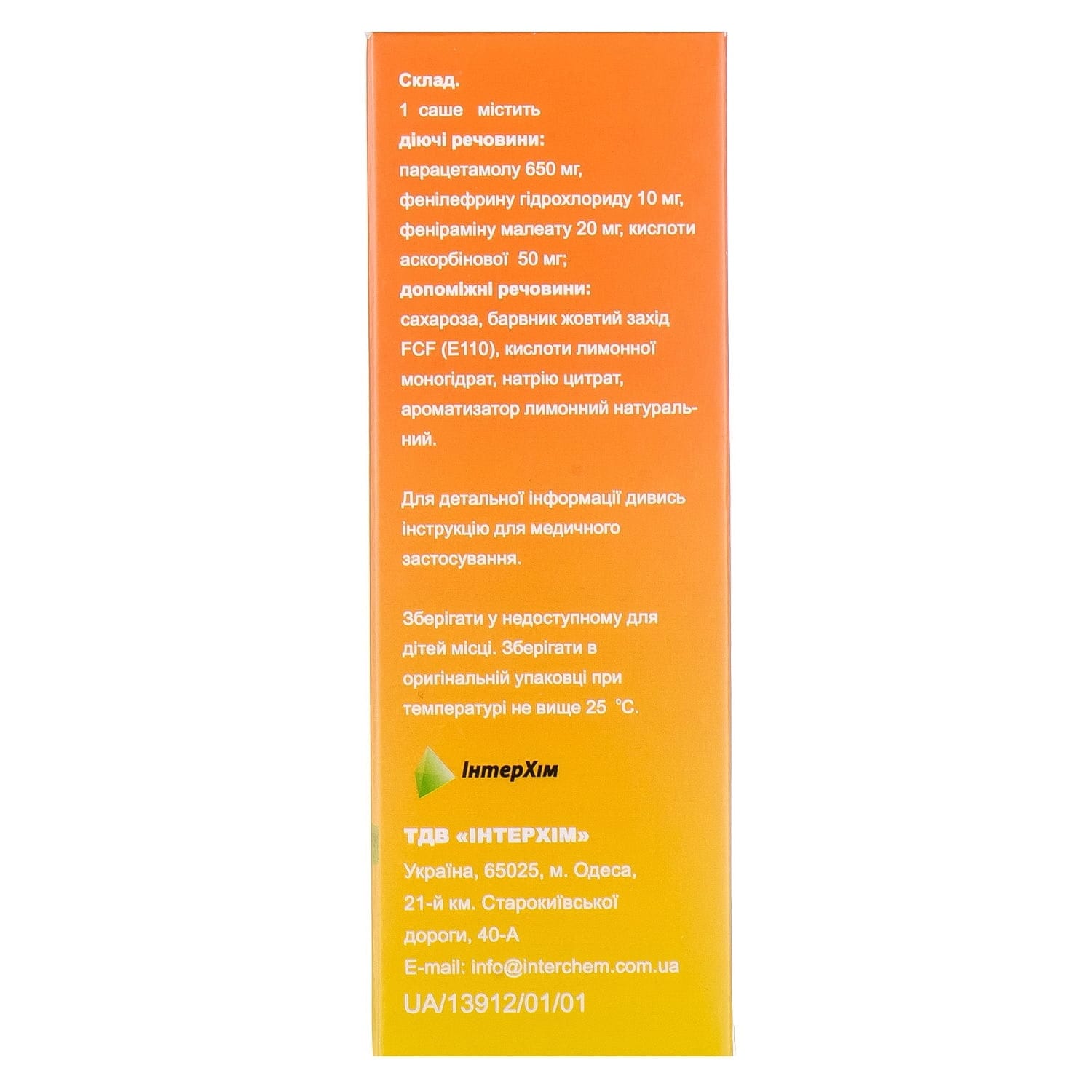
Amitsitron Forte powder for oral solution in sachets of 23 g, 10 pcs.
$22.66
Comprehensive cold and flu relief. Amitsitron Plus reduces fever, pain, nasal congestion, cough, and inflammation for fast recovery and comfort.
Categories: Cold and flu
Brand: InterChem
Pharmacological properties
Pharmacodynamics. Antipyretic, analgesic, antihistamine, vasoconstrictor combined agent, the effect of which is due to the properties of the components that make up its composition.
Paracetamol has antipyretic, analgesic and anti-inflammatory effects. Paracetamol mainly inhibits the synthesis of prostaglandins in the CNS and to a lesser extent affects the peripheral nervous system, blocking the conduction of pain impulses.
Well absorbed, penetrates the placental barrier, enters breast milk in small quantities, is metabolized in the liver, excreted by the kidneys, T ½ – 1-4 hours. Duration of action – 3-4 hours.
Pheniramine is an antihistamine, a blocker of histamine H1 receptors on effector cells, reduces vascular permeability, prevents the development of tissue edema, reduces the severity of local exudative processes, eliminates tearing, itching in the eyes and nose.
Well absorbed, metabolized in the liver, excreted mainly by the kidneys, T ½ – 16-18 hours.
Phenylephrine is a sympathomimetic that mainly stimulates α-adrenergic receptors, has a vasoconstrictor effect, and reduces swelling of the nasal mucosa and paranasal sinuses.
Guaifenesin is an expectorant. It works by increasing the volume and reducing the viscosity of secretions in the trachea and bronchi, which makes it easier to cough up phlegm.
Pharmacokinetics. Paracetamol is rapidly and almost completely absorbed from the gastrointestinal tract. When administered orally, C max in blood plasma is reached 10-60 minutes after administration. 95% of paracetamol is metabolized in the liver by sulfo- and glucuroconjugation, as well as oxidation by the cytochrome P450 system. It is excreted by the kidneys, mainly in the form of metabolites, 3% of paracetamol is excreted unchanged. T ½ is 1-4 hours. Paracetamol penetrates the placental barrier, a small part penetrates into breast milk.
Guaifenesin is rapidly absorbed from the gastrointestinal tract. When administered orally, C max in blood plasma is reached 15 minutes after administration. Guaifenesin is metabolized in the kidneys by oxidation to β-(2-methoxyphenoxy) lactic acid, an inactive metabolite that is excreted in the urine. T ½ is 1 hour.
Phenylephrine hydrochloride is absorbed in the gastrointestinal tract unevenly and undergoes presystemic metabolism by MAO in the intestine and liver. Thus, orally administered phenylephrine has a reduced bioavailability. C max in blood plasma is achieved within 1-2 hours. T ½ is 2-3 hours. It is excreted in the urine almost completely as a sulfate conjugate.
Ascorbic acid compensates for the increased need for vitamin C in respiratory infections, strengthens the body’s nonspecific resistance. It is rapidly absorbed, metabolized in the liver, and excreted by the kidneys.
Indication
Symptomatic treatment of acute respiratory infections and influenza: fever, headache, nasal congestion, runny nose, pain and muscle aches.
For Amitsitron Plus and Amitsitron Plus Sugar-Free preparations also: productive cough with difficult sputum discharge.
Application
The drug is prescribed for adults and children over 14 years of age. It is taken orally in the form of a solution. The contents of the sachet are dissolved in a glass of hot water (not boiling water). It can be taken every 3-4 hours, but no more than 3 sachets per day. The maximum period of use without consulting a doctor is 3 days, further use is on the recommendation of a doctor.
Amitsitron plus and Amitsitron plus without sugar: apply inside in the form of a solution. Dissolve the contents of 1 sachet in 250 ml of hot water, but not boiling water. Use the prepared solution in a warm form. Adult elderly patients, children over 12 years of age: 1 sachet every 4-6 hours if necessary. Maximum daily dose – 4 sachets. Maximum period of use without consulting a doctor – 3 days. If the symptoms of the disease do not disappear, you should consult a doctor. The drugs are contraindicated for children under 12 years of age.
Amitsitron Extratab: adults and children over 12 years of age: 1 tablet every 4 hours. Wash down with water. The maximum daily dose – 6 tablets – should not be exceeded. The maximum period of use without consulting a doctor is 3 days. Further use is possible only under the supervision of a doctor.
Contraindication
Hypersensitivity to the components of the drug; pyloroduodenal obstruction; acute pancreatitis; severe liver and/or kidney dysfunction; congenital hyperbilirubinemia (including Gilbert’s syndrome); glucose-6-phosphate dehydrogenase deficiency; diabetes mellitus; hyperthyroidism; prostatic hypertrophy with urinary retention; bladder neck obstruction; severe forms of arrhythmia, angina pectoris, atherosclerosis, coronary artery disease, blood diseases (including leukopenia, severe anemia); thrombosis; thrombophlebitis; BA; glaucoma; epilepsy; alcoholism, states of increased excitement; concomitant treatment with MAO inhibitors and a period of 2 weeks after their discontinuation.
Amitsitron plus and Amitsitron plus without sugar also: pheochromocytoma, phenylketonuria; rare hereditary problems associated with fructose intolerance, glucose-galactose malabsorption or sucrase-isomaltase insufficiency. Pregnancy and breastfeeding. Age up to 12 years.
Do not use simultaneously with tricyclic antidepressants, paracetamol-containing drugs, β-adrenergic blockers, sympathomimetics.
Side effects
Skin and subcutaneous tissue disorders: dermatitis.
Immune system: anaphylaxis, hypersensitivity reactions, including itching, skin and mucous membrane rashes (usually generalized, erythematous rash, urticaria), angioedema, erythema multiforme exudative (including Stevens-Johnson syndrome), toxic epidermal necrolysis (Lyell’s syndrome).
From the nervous system: headache, dizziness, tremor, psychomotor agitation and disorientation, anxiety, nervous excitability, feeling of fear, irritability, sleep disturbances, insomnia, drowsiness, confusion, hallucinations, depressive states, paresthesias, tinnitus, in some cases – coma, convulsions, dyskinesia, behavioral changes.
On the part of the organ of vision: impaired vision and accommodation, mydriasis, increased intraocular pressure, dry eyes.
Respiratory system: bronchospasm in patients sensitive to acetylsalicylic acid and other nonsteroidal anti-inflammatory drugs.
Gastrointestinal tract: nausea, vomiting, heartburn, dry mouth, discomfort and pain in the epigastric region, constipation, diarrhea, flatulence, aphthae, hypersalivation, hemorrhages.
On the part of the hepatobiliary system: impaired liver function, increased activity of liver enzymes, usually without the development of jaundice, hepatonecrosis (when using high doses).
On the part of the endocrine system: hypoglycemia, up to hypoglycemic coma.
From the urinary system: nephrotoxicity, interstitial nephritis, papillary necrosis, dysuria, urinary retention and difficult urination, aseptic pyuria.
On the part of the cardiovascular system: arterial hypertension, arrhythmias (tachycardia, bradycardia, etc.), shortness of breath, pain in the heart area.
From the blood and lymphatic system: anemia (including hemolytic anemia), sulfhemoglobinemia and methemoglobinemia (cyanosis, shortness of breath, pain in the heart area), thrombocytopenia, agranulocytosis, bleeding, bruising.
Others: general weakness.
Special instructions
Do not exceed the recommended doses. In case of overdose, consult a doctor immediately due to the risk of liver damage, even if the patient feels well.
If you have been told you have an intolerance to some sugars, contact your doctor before taking this medicine. Amitsitrone contains sucrose, so patients with rare hereditary problems of fructose intolerance, glucose-galactose malabsorption or sucrase-isomaltase insufficiency should not take this medicine. Amitsitrone contains sodium, so patients on a controlled sodium diet should take this medicine with caution. The medicine contains sunset yellow FCF (E110), which may cause allergic reactions.
Do not use simultaneously with other drugs intended for the symptomatic treatment of colds and rhinitis (vasoconstrictors, paracetamol-containing). Patients with mild arthritis who take analgesics every day and patients who use warfarin or similar drugs that cause an anticoagulant effect should consult a doctor before using the drug.
Patients with severe infections such as sepsis, which are accompanied by a decrease in glutathione levels, are at increased risk of metabolic acidosis when taking paracetamol. Symptoms of metabolic acidosis include deep, rapid or difficult breathing, nausea, vomiting, loss of appetite. You should seek immediate medical attention if these symptoms occur.
In case of liver or kidney diseases, it is necessary to consult a doctor before using the drug. It should be borne in mind that patients with alcoholic non-cirrhotic liver damage have an increased risk of hepatotoxic effects of paracetamol.
Use with caution in patients with Raynaud’s disease, hypertension, heart disease, arrhythmias (bradycardia, etc.), prostatic hypertrophy, pheochromocytoma, thyroid, liver and kidney diseases, glaucoma, chronic lung diseases and the elderly. The drug contains phenylephrine, which can lead to angina attacks.
The drug may affect the results of laboratory tests for blood glucose and uric acid.
If symptoms persist (especially if the headache becomes persistent), you should consult a doctor.
Long-term use of the drug without consulting a doctor can be dangerous.
Amitsitron Plus and Amitsitron Plus Sugar-Free contain aspartame (E951), a source of phenylalanine, which is dangerous for patients with phenylketonuria.
Use during pregnancy and breastfeeding. Do not use.
Ability to influence the reaction rate when driving or operating other mechanisms. When using Amitsitron, it is not recommended to drive a car or operate other mechanisms, as the drug may cause dizziness and drowsiness.
Interactions
The rate of absorption of paracetamol may increase with the use of metoclopramide and domperidone and decrease with the use of cholestyramine. Barbiturates reduce the severity of the antipyretic effect of paracetamol. Anticonvulsants (including phenytoin, barbiturates, carbamazepine), which stimulate the activity of liver microsomal enzymes, may enhance the toxic effect of paracetamol on the liver due to an increase in the degree of its conversion to hepatotoxic metabolites. With the simultaneous use of paracetamol with hepatotoxic drugs, the toxic effect of drugs on the liver increases. Simultaneous use of paracetamol in high doses with isoniazid increases the risk of developing hepatotoxic syndrome. The anticoagulant effect of warfarin and other coumarins may be enhanced with simultaneous long-term regular daily use of paracetamol with an increased risk of bleeding; periodic administration does not cause a significant effect. Paracetamol reduces the effectiveness of diuretics. Do not use simultaneously with alcohol.
The interaction of phenylephrine with monoamine oxidase inhibitors causes a hypertensive effect, tricyclic antidepressants (amitriptyline) – increases the risk of cardiovascular side effects, digoxin and cardiac glycosides – leads to arrhythmia and heart attack. Phenylephrine with other sympathomimetics increases the risk of adverse cardiovascular reactions, may reduce the effectiveness of β-blockers and antihypertensive drugs (reserpine, methyldopa) with an increased risk of hypertension and adverse cardiovascular reactions.
Pheniramine enhances the anticholinergic effect of atropine, antispasmodics, tricyclic antidepressants, antiparkinsonian drugs. Simultaneous use of pheniramine with hypnotics, barbiturates, sedatives, neuroleptics, tranquilizers, anesthetics, narcotic analgesics, alcohol can significantly increase the severity of its depressing effect.
Ascorbic acid when taken orally enhances the absorption of penicillin, iron, reduces the effectiveness of heparin and indirect anticoagulants, increases the risk of crystalluria in treatment with salicylates and the risk of glaucoma in the treatment of GCS, in high doses reduces the effectiveness of tricyclic antidepressants. Antidepressants, antiparkinsonian and antipsychotic drugs, phenothiazine derivatives increase the risk of urinary retention, dry mouth, constipation. Ascorbic acid can be taken only 2 hours after the injection of deferoxamine, since their simultaneous administration increases iron toxicity, especially in the myocardium. Long-term administration of large doses during treatment with disulfiram inhibits the disulfiram-alcohol reaction.
Guaifenesin enhances the effects of sedatives and muscle relaxants.
Overdose
If the patient has taken the drug in a dose exceeding the recommended dose, a doctor should be consulted immediately due to the risk of liver damage. Liver damage is possible in adults who have taken ≥10 g of paracetamol, and in children who have taken paracetamol in a dose of 150 mg/kg of body weight. Taking ≥5 g of paracetamol can lead to liver damage in patients with risk factors (long-term use of carbamazepine, phenobarbital, phenytoin, primidone, rifampicin, St. John’s wort or other drugs that induce liver enzymes, regular excessive alcohol consumption; insufficiency of the glutathione system, such as eating disorders, HIV infection, starvation, cystic fibrosis, cachexia).
Symptoms of paracetamol overdose in the first 24 hours: pallor, nausea, vomiting, loss of appetite and abdominal pain. Liver damage may become apparent 12-48 hours after overdose. Glucose metabolism disorders and metabolic acidosis may occur. In severe poisoning, liver failure may progress to encephalopathy, hemorrhage, hypoglycemia, coma and death. AKI with acute tubular necrosis may present with severe lower back pain, hematuria, proteinuria and may develop even in the absence of severe liver damage. Cardiac arrhythmias and pancreatitis have also been reported.
With prolonged use of paracetamol in high doses, aplastic anemia, pancytopenia, agranulocytosis, leukopenia (including neutropenia), thrombocytopenia may develop from the hematopoietic system. When taken in high doses, dizziness, psychomotor agitation, disorientation, sleep disturbances are possible from the CNS; from the urinary system – nephrotoxicity (renal colic, interstitial nephritis, papillary necrosis) is possible.
In case of overdose, urgent medical attention is required. The patient should be taken to hospital immediately, even if there are no early symptoms of overdose. Symptoms may be limited to nausea and vomiting or may not reflect the severity of the overdose or may lead to organ damage. Treatment with activated charcoal should be considered if an overdose of paracetamol has been taken within 1 hour. The concentration of paracetamol in the blood plasma should be measured 4 hours or later after ingestion (earlier concentrations are unreliable). Treatment with N-acetylcysteine can be used within 24 hours of paracetamol ingestion, but the maximum protective effect occurs when it is used within 8 hours of ingestion. The effectiveness of the antidote decreases sharply after this time. If necessary, the patient should be given N-acetylcysteine intravenously according to current recommendations. In the absence of vomiting, oral methionine can be used as a suitable alternative in remote areas outside the hospital.
Overdose of phenylephrine causes hyperhidrosis, psychomotor agitation or depression of the central nervous system, headache, dizziness, drowsiness, impaired consciousness, arrhythmias, tremor, hyperreflexia, convulsions, nausea, vomiting, irritability, anxiety, and hypertension.
In case of an overdose of pheniramine, atropine-like symptoms occur: mydriasis, photophobia, dryness of the skin and mucous membranes, hyperthermia, intestinal atony. CNS depression leads to disruption of the respiratory and cardiovascular systems (bradycardia, arterial hypotension, collapse).
An overdose of ascorbic acid causes nausea, vomiting, bloating and abdominal pain, itching, skin rashes, increased excitability. Doses of 3000 mg can cause temporary osmotic diarrhea and gastrointestinal disorders, zinc and copper metabolism disorders, myocardial dystrophy, glucosuria, crystalluria, nephrolithiasis.
Guaifenesin. Overdose in small or moderate doses may cause dizziness or vertigo, gastrointestinal disturbances (including nausea, vomiting). Very high doses may cause symptoms such as agitation, confusion, and respiratory depression.
Treatment: symptomatic therapy. Within 6 hours after overdose, gastric lavage should be performed, and within the first 8 hours, methionine should be administered orally or cysteamine or N-acetylcysteine should be administered intravenously.
Storage conditions
In the original packaging at a temperature not exceeding 25 °C.
Be the first to review “Amitsitron Forte powder for oral solution in sachets of 23 g, 10 pcs.” Cancel reply
You may also like










Reviews
There are no reviews yet.